Of Bacteria and Bad Actors
FDA scientists, like Diane Biron, must battle both to ensure the safety of America’s medical devices.
lab cleanroom, prepares to test bandages
and insulin syringes for sterility.
Diane Biron is a bacteria hunter. But she’s not focused on the obvious microbial hideaways, like grimy nooks and crannies touched by countless strangers. Instead, it’s new, shiny, hard surfaces, presumably germ-free, that concern her.
In her Boston-area laboratory, suited up most days from head to toe in a hooded coverall, mask, and gloves, Biron scrutinizes medical devices for the presence of potentially killer pathogens. The list of bad guy bacteria she stalks, through her use of various detection tests, are a brutal lot, capable of causing deadly infections, while posing stubborn resistance to entire arsenals of antibiotics. Such bacteria include the headline-grabbing E. coli, as well as lesser known Burkholderia cepacia and Pseudomonas aeruginosa, both responsible for thousands of hospital patient infections, some fatal, each year.
This lab work can be intense, particularly during public health emergencies when it’s Biron’s job to pinpoint which of the many microbial suspects, potentially associated with an illness-causing medical device or other product, is making people sick. Her swift ID opens the door to appropriate patient treatments and other public-protecting actions by the agency.
But the search isn’t straightforward. Adding to the challenge is what Biron, now in her ninth year at the FDA, must search for: bits of bacteria “skin.” Hardly benign sheddings, these poisonous molecules are produced by pathogens responsible for some of the world’s deadliest outbreaks.
Sophisticated Foes
serious sterility issues associated with stents, such
as this one, meant to treat narrowing blood vessels.
Already menacing, some bacteria—like those that cause plague, cholera, and whooping cough—will release potent molecules, called endotoxins, when their cells rupture, face death, or alternatively, are multiplying vigorously. “Fortunately, our immune system has evolved to recognize these toxins as a threat and to react accordingly,” says Biron. The body’s response, typically fever and diarrhea, while temporarily uncomfortable, is usually effective at halting further harm. But if endotoxins continue to build up in the blood in a condition known as endotoxemia--hypotension, respiratory failure, and reduced oxygen delivery can result. “Taken further, strong endotoxemia can lead to sepsis,” adds Biron, “and eventually death.”
What makes endotoxins additionally vexing for public health microbiologists is their uncanny ability to fly under the radar. That means Biron and her colleagues must intentionally, and intently, be looking for the toxins to even find them. Furthermore, a surface can be deemed “sterile,” yet still be contaminated with what she calls “low-level” endotoxins.
Naturally, this is a serious concern for health scientists, doctors, patients, or really anyone who relies on or comes into contact with a medical device. And as bacterially released endotoxins can lurk almost anywhere in our environment, they threaten to contaminate medical devices and drugs, even those fresh from a manufacturing facility—especially if sterility measures are not up to snuff. And a compromised medical device, particularly one implanted into a patient—such as a cardiac stent, or a neural/ brain tissue repair implant—can cause entirely unintended and devastating consequences.
Sterility, Deconstructed
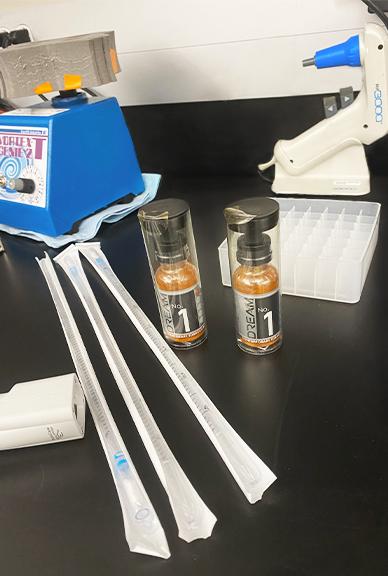
Approximately 50 mason jars filled with clear fluids sit on a counter in Biron’s highly controlled cleanroom at the FDA’s Winchester Engineering and Analytical Center (WEAC). Inside the jars are bits and pieces of catheter tubing, diabetic lancets, bandages, and hospital syringes—medical devices all purporting to be “sterile.” But Biron, as her job requires, can’t make any assumptions about their degree of cleanliness. Instead, she must be relentlessly suspicious of products she evaluates, given the potential impacts on public health. Only her blue eyes showing from beneath her white hood, she forcefully cuts apart a clear-tubed catheter—trimming off plastic caps and joints with the abandon a curious child might enjoy while dismantling a toy.
Because medical devices vary greatly in size—from contact lenses and adhesive bandages (yes, they’re treated as medical devices by the FDA who oversees their safety, too) to IV bags, cardiac ablation electrodes, transplant organ tissue fluid, trachea tubing, hospital syringes, and many others—regulatory scientists focused on sterility and safety must often disassemble devices, or break them up into smaller fragments, however creatively they must, to achieve a thorough examination.
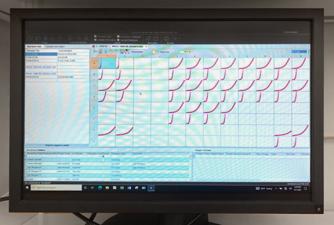
On this day, Biron is examining vials containing samples of jar solutions that have been treated to a 14-day incubation, equally split between two incubating temperatures, 32.5 degrees Celsius (or 90.5 degrees Fahrenheit) and room temperature. She holds one of the vials up to the light. Its once-clear fluid contents have turned milky white. Cloudiness, or turbidity, is evident—a tell-tale sign that bacterial or fungal contamination is present.
The test has its limits though. It can't detect endotoxins released when gram negative bacteria die, so for that, Biron relies on two other specialized tests: the kinetic assay and gel-clot assay. Used by scientists worldwide for endotoxin detection, these assays can zero in on lifeless, but still dangerous, endotoxins. Curiously, their detection powers rely on a vibrantly colored blood source from one of Earth’s most primitive organisms.
A Blue Blood Intervention
Back in the 1960’s, in Woods Hole, Mass., coincidentally only about an hour-and-a-half drive from FDA’s current WEAC facility, marine biologist Frederick Bang was studying the circulatory system of the Atlantic horseshoe crab when he made a stunning discovery. Bang, with the support of eventual colleague Jack Levin, found that when the blood of the horseshoe crab—already distinctive because of its striking Mediterranean-blue color (a result of copper, not iron, pigments in the creature’s blood)—was confronted with harmful gram-negative bacteria, like E. coli, the crab’s blood cells promptly coagulated. This was the animal’s way to barricade its circulatory system against further harm.
This finding—basic research eventually leveraged for a specific and powerful medical application—has become the basis for the endotoxin tests still considered the gold standard today. Called the Limulus Amebocyte Lysate, or LAL, test (Limulus in reference to the crab’s genus, and amebocyte, the name of its blood cell), the assay exists in a few forms. There’s the gel-clot test, in which an analyst assesses a sample for the same kind of coagulation, or congealing, that Bang and Levin observed years ago in the crab’s blood. There’s also the chromogenic test that uses visible color changes—specifically, a solution turns bright yellow—when in the presence of harmful bacteria.
These tests, harnessing a sophisticated animal adaptation likely millions of years in the making, are vital to Biron and her colleagues’ work. “The kinetic assay derived from the horseshoe crab blood was vital to WEAC’s testing of Ophthalmic Viscosurgical Devices (OVDs), during several adverse health outbreaks involving suspected contaminated OVDs used during cataract surgery.”
The tests are also illustrative of the basic research that lies at the heart of next-generation science--much needed at public institutions like the FDA, for its promise to patient health and in meeting the public health challenges we’ll invariably face in the future.
Noncompliance
drug API (active pharmaceutical ingredients)
Unfortunately, it’s not just dodgy pathogens that Biron must pursue. She and her colleagues are also tasked with helping uncover the insufficient practices of device manufacturers who don’t follow sterility rules.
The FDA enforces the Code of Federal Regulations, or CFR, as it relates to medical products—through regular onsite visits by consumer safety officers to manufacturing facilities, among other activities. These visits, in which Biron participates too, verify that a firm’s strategy for microbial testing and its quality controls—including the type, frequency, as well as the endotoxin limits associated with a specific medical device—are adequate for ensuring a safe product.
This is crucial considering that even the most pristine manufacturing environments can become compromised—whether from exposure to pathogens in water or air (ventilation) sources, or through good old-fashioned human contact in the production line. And robust sterility practices become even more compelling when conducted in support of medical devices or implants designed to be used in direct contact with a patient’s blood, lymphatic, or cerebrospinal fluids.
Still, sadly, profit-over-safety motivations exist. That’s why regulatory scientists like Biron, with expertise in disciplines like chemistry and microbiology, must also be adept at sleuthing serious device manufacturing deficiencies and providing evidence, ready to stand up in a court of law, that a firm lacks appropriate safeguards—or, in some cases, is willfully disregarding the agency’s scientifically based regulations.
She and her consumer safety officer colleagues have done this before—their findings leading to firms halting their manufacturing processes and recalling faulty or compromised devices. The FDA’s overarching intent is simple: to keep unsafe medical products from ever reaching the public.
“It’s shocking really, with regulations so easily accessible to device manufacturers, that we still find unsafe devices making their way to hospitals,” say Biron. “But that’s what we’re here for, to keep those dubious firms in check.”
Thanks to the efforts of vigilant regulatory researchers and their investigator colleagues—as well as a bevy of industry partners who do, in fact, care deeply about patient safety alongside innovation, U.S. patients can take for granted that the artificial knee implant, cardiac stent, or other medical device they’re in need of will be safe. Patients can instead focus their energies on recovery and getting back to their everyday lives.