2021 FDA Science Forum
Dosing Strategy of Immunoglobulins (IgG) Replacement Therapies in Obese and Overweight Patients with Primary Immunodeficiency Diseases (PIDDs)
- Authors:
- Center:
-
Contributing OfficeCenter for Biologics Evaluation and Research
Abstract
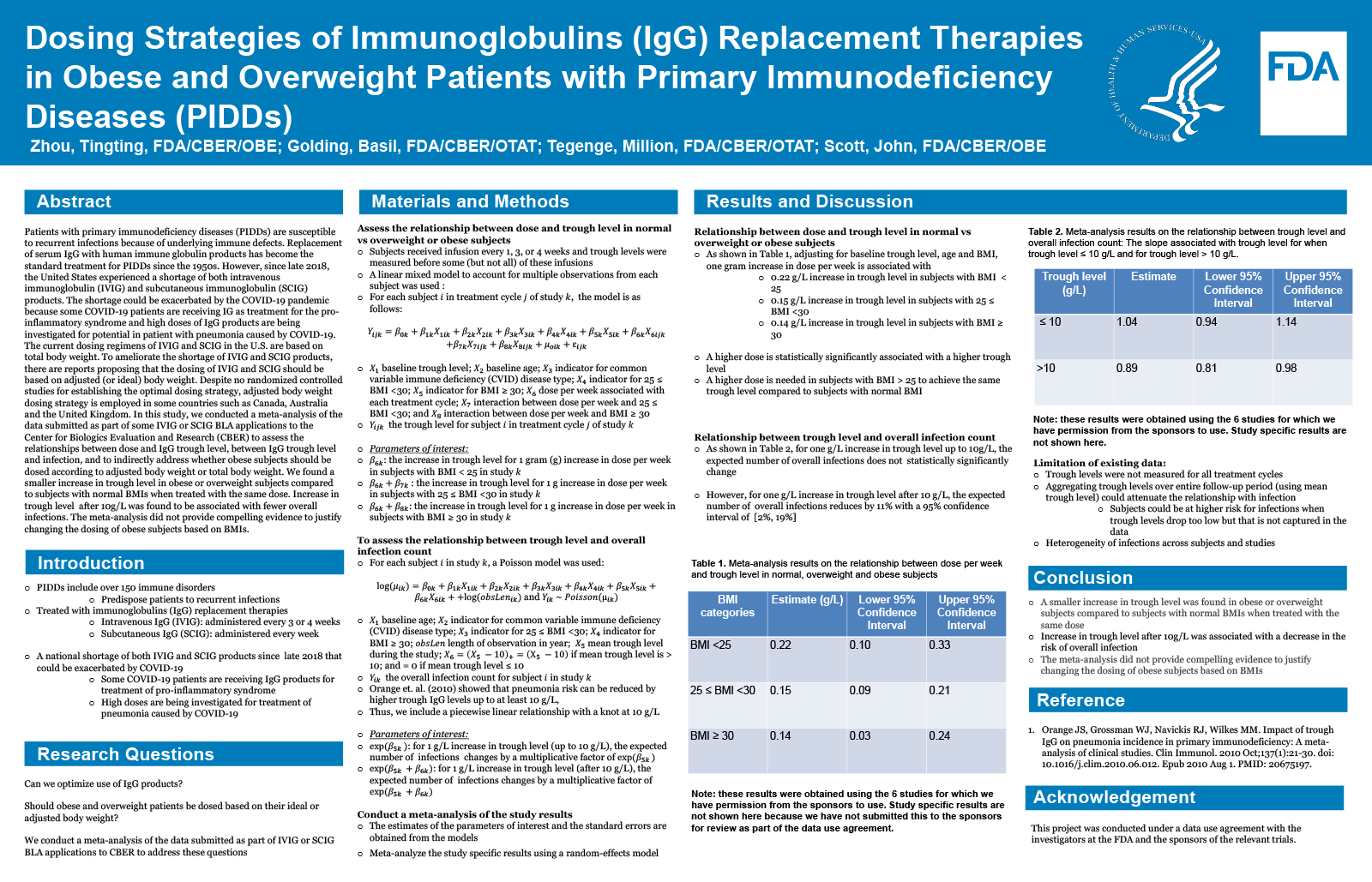
Patients with primary immunodeficiency diseases (PIDDs) are susceptible to recurrent infections because of underlying immune defects. Replacement of serum IgG with human immune globulin products has become the standard treatment for PIDDs since the 1950s. However, since late 2018, the United States (U.S.) experienced a shortage of both intravenous immunoglobulin (IVIG) and subcutaneous immunoglobulin (SCIG) products. The shortage could be exacerbated by the COVID-19 pandemic because some COVID-19 patients are receiving IG as treatment for the pro-inflammatory syndrome and high doses of IgG products are being investigated for potential in patient with pneumonia caused by COVID-19. The current dosing regimens of IVIG and SCIG in the U.S. are based on total body weight. To ameliorate the shortage of IVIG and SCIG products, there are reports proposing that the dosing of IVIG and SCIG should be based on adjusted (or ideal) body weight. Despite no randomized controlled studies establishing the optimal dosing strategy, adjusted body weight dosing strategy is the standard practice in some countries such as Canada, Australia and the United Kingdom. In this study, we conducted a meta-analysis of the data submitted as part of some IVIG or SCIG BLA applications submitted to the Center for Biologics Evaluation and Research (CBER) to assess the relationships between dose and IgG trough level, between IgG trough level and infection, and to indirectly address whether obese subjects should be dosed according to adjusted body weight or total body weight. We found a smaller increase in trough level in obese or overweight subjects compared to subjects with normal BMIs when treated with the same dose. A small increase in trough level in obese subjects was found to be associated, but not statistically significantly, with fewer overall infections. The meta-analysis did not provide compelling evidence to justify changing the dosing of obese subjects based on BMIs.