Sickle Cell Disease: A Spotlight on Women
Knowledge and News on Women’s Health (KNOWH) blog from FDA Office of Women’s Health

September is National Sickle Cell Awareness Month. This annual observance helps raise awareness about sickle cell disease (SCD) and spotlights ongoing advancements in research and treatment options for those who are living with this chronic and often painful disease. SCD is the most common inherited blood disorder and affects approximately 100,000 Americans.
OWH invited Titilope Fasipe, MD, PhD., Co-Director, Sickle Cell & Thalassemia Program Texas Children’s Hospital, to guest author and share her insights and expertise for our special OWH blog post on sickle cell disease in women.
The views expressed are those of Dr. Fasipe and do not necessarily reflect the opinions, views, or official policy of the U.S. Food and Drug Administration’s Office of Women’s Health.
1. What is sickle cell disease and what causes it?
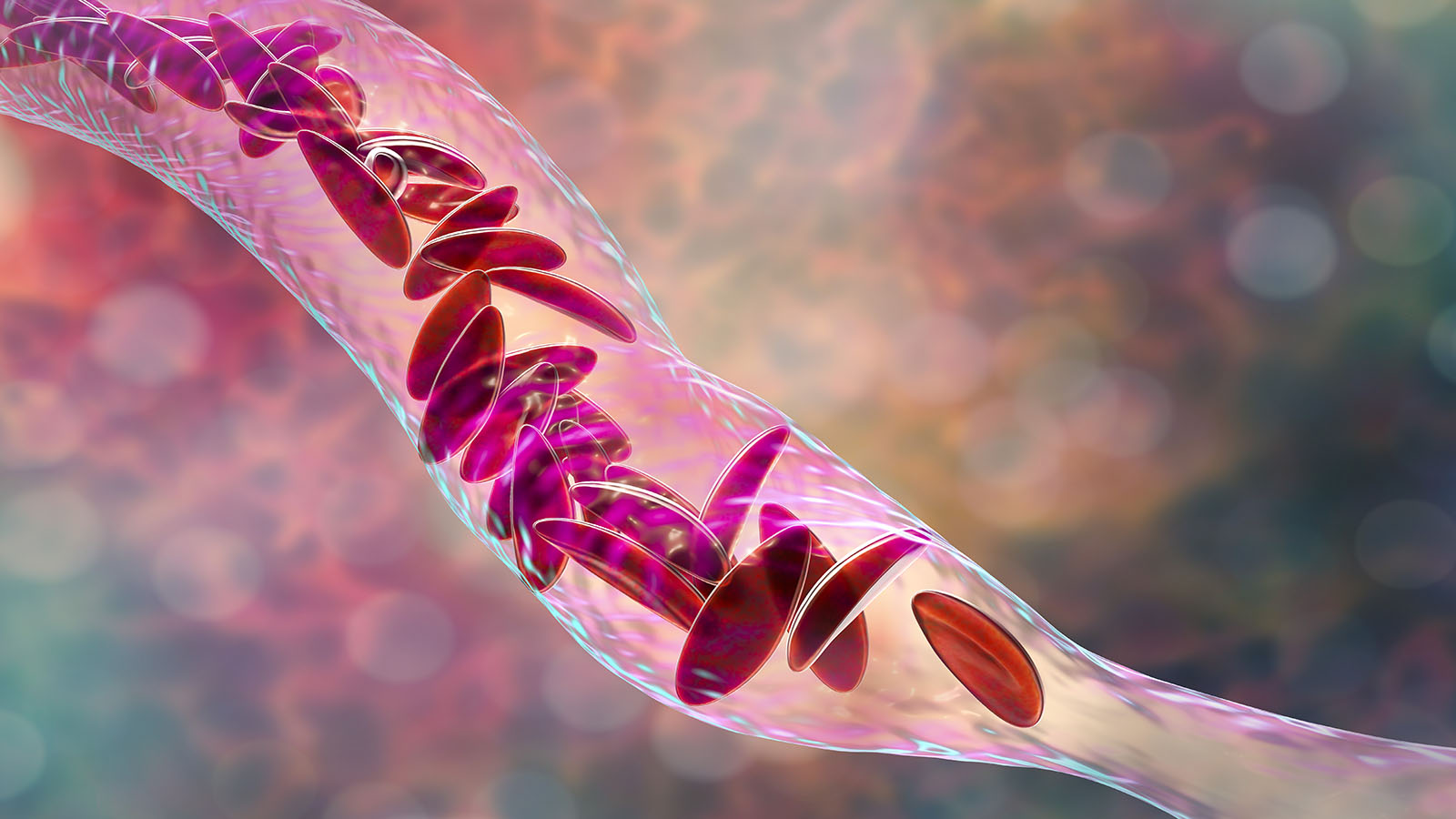
Sickle cell disease is an inherited blood disorder that affects hemoglobin, the protein that carries oxygen through the body. SCD is caused when a person inherits two mutations in hemoglobin genes—one from each parent—leading to a faulty hemoglobin protein called hemoglobin S. Red blood cells are normally disc-shaped and flexible to allow them to move easily through the blood vessels. When a person has SCD, their red blood cells become crescent or “sickle” shaped due to the genetic mutation. These “sickle” shaped cells are not as flexible and can block blood flow to the rest of the body. SCD is a lifelong health condition that can cause anemia, severe pain, and organ damage.
2. Are all newborns screened for sickle cell disease?
Since 2006, all newborns in the United States are screened for SCD as part of each state’s newborn screening program. However, every country does not necessarily screen for SCD, including many countries with higher birth rates of SCD than the US.
3. Are there certain populations or ethnic groups who are at higher risk for sickle cell disease?
Yes, Black or African American and Hispanic or Latino Americans have a higher risk of being born with SCD. In fact, about 1 out of every 400 Black or African Americans and about 1 out of every 16,000 Hispanic/Latino Americans are born with SCD. The sickle cell/HbS mutation is thought to have originated on the continent of Africa thousands of years ago. Most people with SCD are of sub-Saharan African, Indian, or Middle Eastern descent. Due to the Trans-Atlantic slave trade and migration, a person with SCD can be of any ethnicity.
4. What are the symptoms of sickle cell disease?
Sickle cell disease affects the hemoglobin in red blood cells and because red blood cells flow throughout the blood vessels in the body, complications of SCD can occur anywhere in the body. Common symptoms include fatigue due to the anemia, and excruciating pain episodes as a result of blockage of blood vessels and jaundice, a condition where a person’s skin and the whites of their eyes can turn yellow. The symptoms and complications of SCD can vary in severity from person to person and may change over time.
5. What are the major complications of sickle cell disease?
Major complications include cognitive dysfunction, stroke, acute chest syndrome, acute and chronic pain, chronic bone damage, delayed growth/puberty, increased risk of infections, gallstones, kidney disease, blood clots (deep venous thrombosis), sickle cell retinopathy (eye disease), and shortened lifespan.
6. Are there any effective treatments for sickle cell disease? Is there a cure?
FDA-approved treatments for SCD include hydroxyurea, L-glutamine, crizanlizumab, and voxelotor. These medicines can help people living with SCD in different ways, such as:
- By reducing the risk of red blood cells becoming “sickled”;
- Improving blood flow and how well red blood cells work;
- Decreasing pain, inflammation, and damage to blood vessels;
- Reducing the complications of SCD.
Transfusions are also sometimes used to manage SCD complications. A potentially curative approach for SCD is a stem cell transplant. Moreover, the FDA recently approved two types of gene therapy.
Speak with your health care provider about which treatment options may be best for you.
7. How does sickle cell disease impact women, and are there any precautions women with sickle cell disease should consider if they are planning to become pregnant?
Sickle cell disease impacts women in various ways. It may cause delayed puberty and is also associated with reproductive complications, including preeclampsia and infants with low birth weight. Pregnancy may also trigger or worsen other sickle cell complications, including pain episodes, acute chest syndrome, blood clots in the legs and lungs (deep vein thrombosis, and pulmonary embolism). If you have SCD, talk with your health care provider about the potential for complications during your pregnancy and any other concerns you may have.
8. Are there any lifestyle routines people living with sickle cell disease should follow to help them live healthier?
A healthy lifestyle routine that includes eating nutritious food and exercising can help improve the quality of life for people living with SCD. It is also important to receive comprehensive care from a hematologist (a doctor who has special training in diagnosing and treating blood disorders), a primary care physician, and other specialists as needed.
9. What research is being done on sickle cell disease?
There is a lot of ongoing research related to SCD including:
- Research on various new drugs, including some in clinical trials.
- Research into gene therapies and stem cell transplants.
- Psychosocial and behavioral research.
- Implementation science research, such as research to help identify and overcome patient barriers and to better train health care providers effectively.
- Quality improvement research such as that which aims to improve health care professional knowledge, workflow, and patient safety.
10. How can I help the people in my life who are living with sickle cell disease?
There are many ways to help people living with SCD:
- Offer support, such as assistance with pain management, preventing complications, and reducing hospitalizations, to help improve their quality of life.
- Consider being a blood or stem cell donor.
- Volunteer/partner with sickle cell community-based organizations and learn how you can support their programs and initiatives.
- Learn more about sickle cell disease, share educational resources, and help raise awareness in your community.
For resources and materials on other women’s health topics, visit www.fda.gov/womens.