2023 FDA Science Forum
Toxicity of three antisense oligonucleotide drugs and eighteen of their impurities in primary human hepatocytes
- Authors:
- Center:
-
Contributing OfficeNational Center for Toxicological Research
Abstract
Background:
Antisense oligonucleotide (ASO) drugs are synthetic polymers of RNA, DNA, or modified nucleic acids that bind to RNA or protein targets, regulating protein expression or function. Though approximately 20 ASOs have been approved around the globe, quality control and safety assessment pose significant challenges to regulatory agencies, with hepatotoxicity associated with many ASOs.
Purpose:
This study uses pooled primary human hepatocytes (p-PHHs), a commonly used in vitro model for drug hepatotoxicity, to assess the potential for increased risk of hepatotoxicity with ASO impurities compared to the parent compounds.
Methodology:
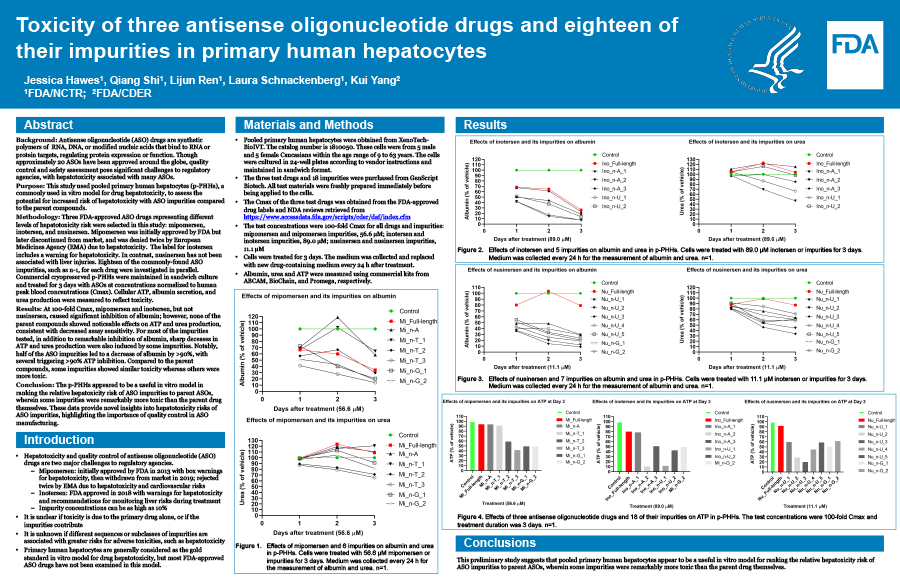
Three FDA-approved ASO drugs representing different levels of hepatotoxicity risk were selected in this study: mipomersen, inotersen, and nusinersen. Mipomersen was initially approved by FDA but later discontinued from market, and was denied twice by European Medicines Agency (EMA) due to hepatotoxicity. The label for inotersen includes a warning for hepatotoxicity. In contrast, nusinersen has not been associated with liver injuries. Eighteen of the commonly-found ASO impurities, such as n-1, for each drug were investigated in parallel. Commercial cryopreserved p-PHHs were maintained in sandwich culture and treated for 3 days with ASOs at concentrations normalized to human peak blood concentrations (Cmax). Cellular ATP, albumin secretion, and urea production were measured to reflect toxicity.
Results:
At 100-fold Cmax, mipomersen and inotersen, but not nusinersen, caused significant inhibition of albumin; however, none of the parent compounds showed noticeable effects on ATP and urea production. Most of the impurities tested caused remarkable inhibition of albumin; whereas sharp deceases in ATP and urea production were induced by some impurities, consistent with decreased assay sensitivity. Notably, half of the ASO impurities led to a decrease of albumin by >90%, with several triggering >90% ATP inhibition. Compared to the parent compounds, some impurities showed similar toxicity whereas others were more toxic.
Conclusion:
The p-PHHs appeared to be a useful in vitro model in ranking the relative hepatoxicity risk of ASO impurities to parent ASOs, wherein some impurities were remarkably more toxic than the parent drug themselves. These data provide novel insights into hepatotoxicity risks of ASO impurities, highlighting the importance of quality control in ASO manufacturing.